AI in Healthcare: Pros, Cons, and Implementation Best Practices
The integration of artificial intelligence (AI) in the healthcare industry has the potential to change the outcomes for patients, associates, and the overall operation. This post shares a high-level overview of the advantages and limitations of AI and explores what questions to ask when considering use cases for AI solutions.
Advantages
- Early diagnoses: By analyzing large amounts of data, AI can assist clinicians with making early diagnoses, which is crucial for precision medicine and predictive analysis. This is particularly exciting for fields like oncology, as AI can help screen symptomatic and asymptomatic patients and analyze the risk of cancer recurrence.
- Personalized medicine: AI can assist with identifying the best treatment options for individual patients based on their genetic and medical data, the systematic analysis of data on prior patient outcomes, and the combined knowledge of thousands of doctors.
- Virtual care and access to care: Organizations are making more services available to patients on digital platforms. AI-powered virtual assistants and chatbots can provide 24/7 support to patients, answer questions and provide information, and even make some common diagnoses without the need for a doctor. This makes healthcare more accessible while reducing the workload of healthcare professionals.
- Clinical trial optimization: AI can assist with the recruitment of patients for clinical trials, predict patient outcomes, and identify potential side effects, which can accelerate the drug development process.
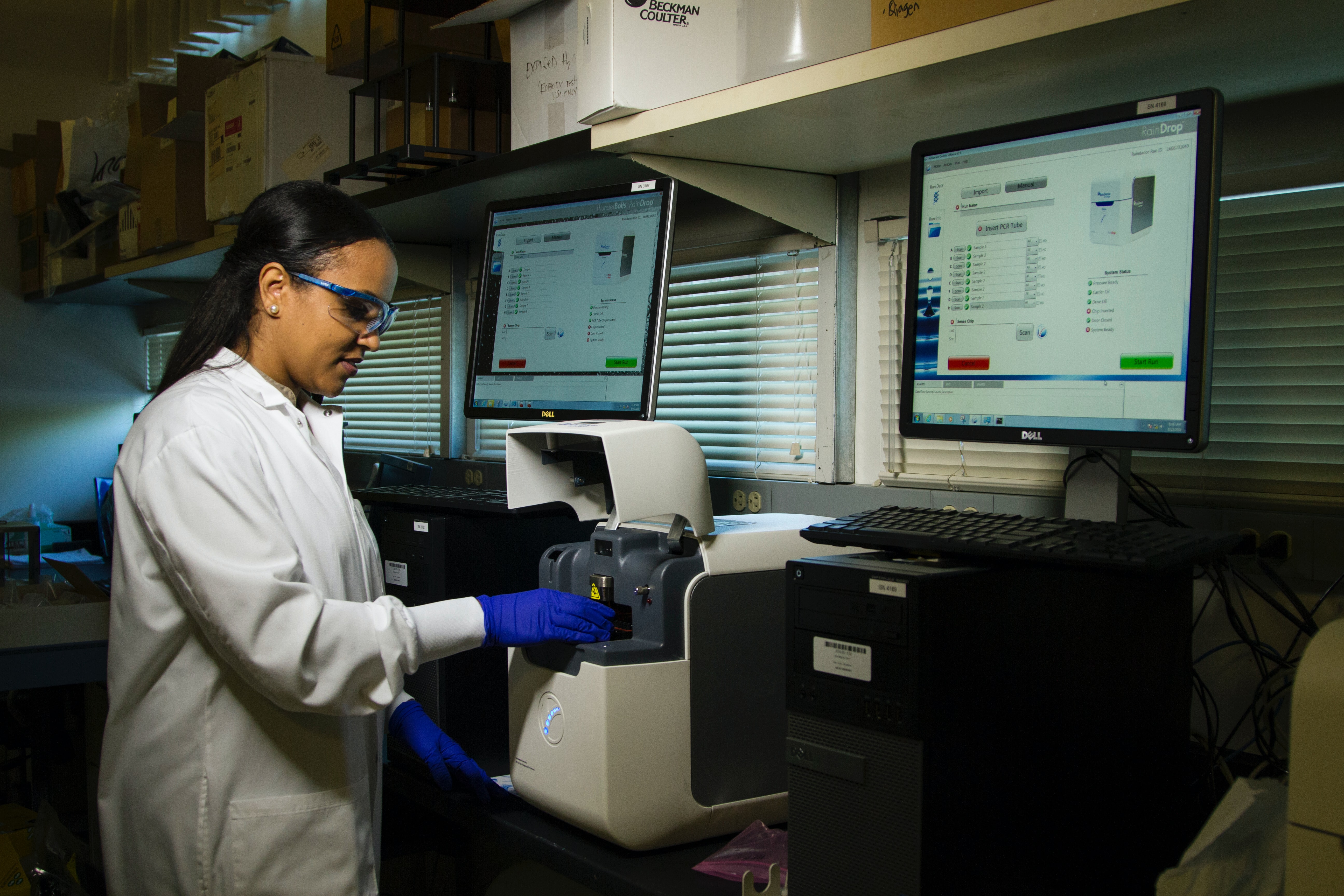
- Accurate testing: Using advanced machine learning (ML) algorithms, AI can analyze test results and medical images with a high degree of accuracy, reducing the risk of human errors. This not only increases the efficiency of healthcare professionals but also allows them to focus on more empathetic interactions and value-added tasks such as patient diagnosis and treatment planning.
- Predictive patient retention: AI and ML-based solutions can analyze patient data and identify patterns of behavior, providing insights on potential reasons for patient attrition. This can assist healthcare providers in creating targeted retention strategies, such as addressing specific concerns, offering personalized incentives to at-risk patients, and identifying weaknesses in the services provided.
- Patient flow and bed management: AI-powered algorithms can provide a comprehensive understanding of patient flow and bed utilization, which can assist in identifying bottlenecks in the system. With real-time visibility of these metrics, providers can take proactive measures to reduce wait times, alleviate overcrowding, prepare for future demand, and adjust staffing levels accordingly. Additionally, AI can assist with predicting patient demand to help proactively manage the availability of beds, resources, and staff, ensuring that patients receive timely and efficient care.
Limitations and complexities
- Ethical standards: Healthcare organizations have access to some of the most sensitive data on earth, raising ethical questions if it falls into the wrong hands. As they increase their leverage of AI, it’s their responsibility to ensure increased security diligence, stay current with laws and regulations, and regularly review and update security practices as threats evolve. This can be costly, but so is putting sensitive patient data at risk. Regardless, organizations can offset this cost by selecting only the best, high-return use cases for AI.
- Data management: Healthcare organizations face unique challenges when it comes to managing and utilizing data, as it requires specialized knowledge in areas such as data categorization, tagging, and machine learning. This can be a significant challenge for organizations, as there may be a shortage of resources with the necessary technical and functional knowledge to effectively manage and utilize healthcare data. Additionally, the large amount of data generated in healthcare can be overwhelming, making it difficult to effectively process, store, and analyze it. Organizations may need to invest in data management infrastructure and technologies, and find specialized personnel to overcome these challenges.
- Physical and digital security: Empowering associates and patients with AI means data is being manipulated regularly in the cloud and on-premises environments serving several front-and back-end platforms. Organizations must carefully select key users of the systems, install physical access controls, and implement new cybersecurity frameworks and encryption tools to protect against external threats.
Questions to ask when exploring use cases for AI in healthcare
- Will it help, or replace? The best health outcomes are achieved with better doctor-patient communication. AI algorithms can aid doctors in making diagnoses and treatment decisions, but they cannot replace the empathy of a healthcare professional.
- Can it streamline processes? By identifying areas of opportunity in patient-facing and backend processes, organizations can use AI to make healthcare more efficient and cost-effective. This can include automating tasks such as appointment scheduling, medication management, and lab results analysis.
- Can it enable new discoveries? By automating repetitive tasks and drawing insights from large amounts of data that may not be apparent to the human eye, organizations AI can accelerate the pace of research and development, identify new drug targets, predict disease outcomes, and more.
- How will it be integrated into existing and future systems and processes? Organizations must consider not only the technical aspects of integration, such as compatibility with existing software and hardware, but also the operational aspects, such as how the solution will fit into the existing workflow and how it will be used by clinicians. Additionally, it’s important to have a clear understanding of the ownership, maintenance, and cost of the solution to ensure that there are enough resources to maintain and update it.
- What are the ethical implications? Any AI solution should comply with relevant regulations and have robust data security measures in place to protect patient privacy. In addition, organizations should consider potential biases in the data used to train AI models and the potential for AI to make decisions that may have negative consequences for patients or specific populations.
- How will it be monitored and evaluated? It’s crucial to have KPIs and other performance metrics in place for any AI solution to measure its success and identify areas for improvement.
Conclusion
The potential for AI in the healthcare industry is vast and new use cases pop up every day. While there are limitations and complexities to consider, the future for this intersection between AI and medicine is promising and one to be eagerly anticipated— so long as the industry focuses on finding practical use cases while overcoming the limitations.
Shannon Helms is a seasoned Business Development Manager for Softtek's Healthcare and Insurance vertical. She brings a wealth of experience and expertise to her clients, offering objective counsel and guidance to drive positive impact and achieve organizational goals. Shannon and her team specialize in the healthcare ecosystem, providing solutions for health systems, payors, and patient delivery. Learn how Softtek is revolutionizing the healthcare industry and connect with our experts by visiting our dedicated healthcare page.


